In Vitro Fertilization (IVF) has emerged as a beacon of hope for many individuals and couples grappling with infertility. This intricate medical procedure transcends the conventional boundaries of reproduction, propelling the journey from longing to fulfillment. However, as with any medical intervention, understanding the nuances—especially the cut-off points—can be daunting. This article aims to demystify IVF, exploring its mechanisms, risks, age considerations, and the essential knowledge required for potential candidates.
The Fundamentals of IVF
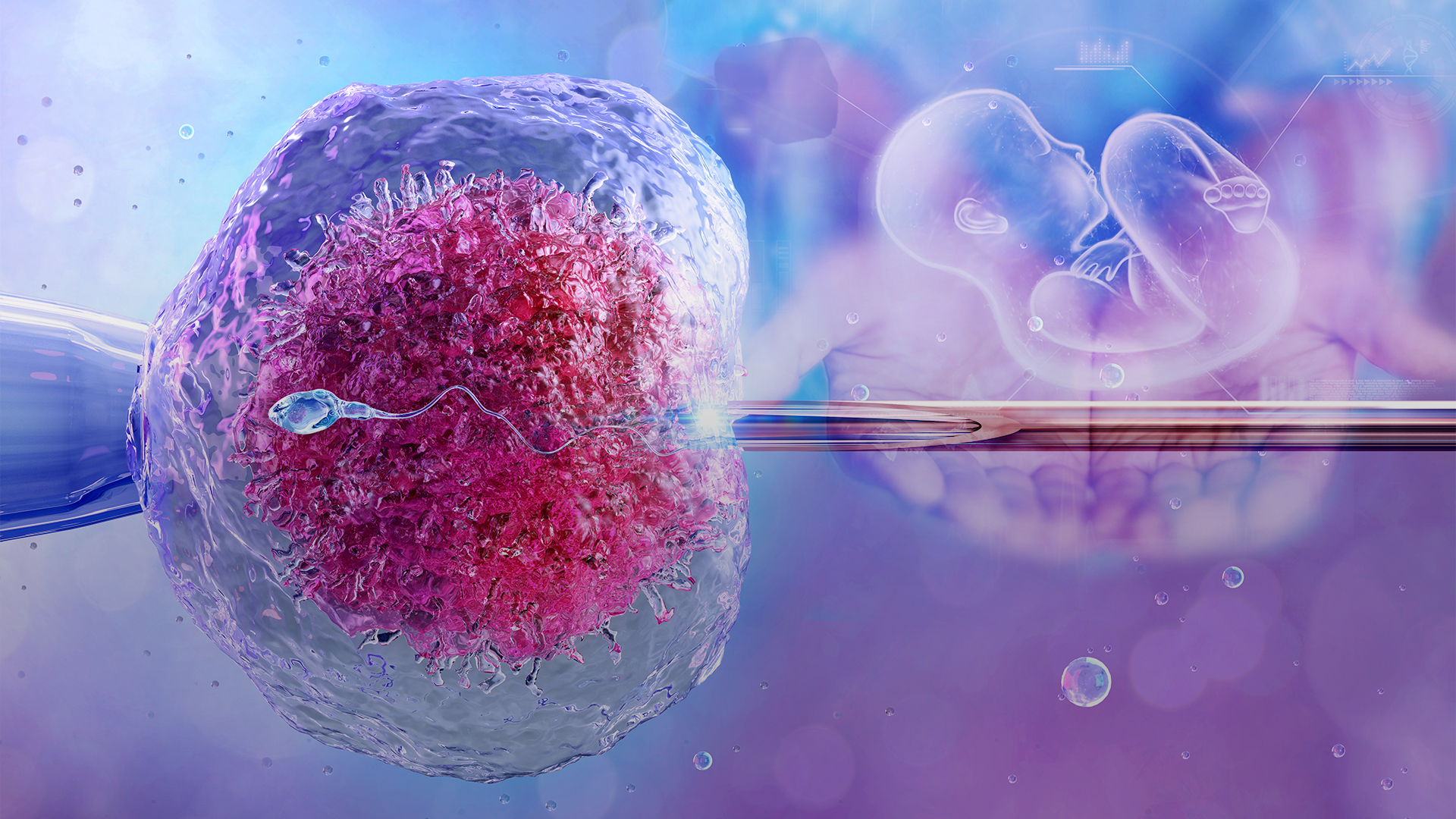
IVF is a multifaceted process where an ovum is fertilized by sperm outside the body, in a controlled laboratory environment. This procedure comprises several key stages, beginning with ovarian stimulation. Hormonal injections are administered to stimulate the ovaries to produce multiple eggs, enhancing the chances of successful fertilization. Following this, egg retrieval occurs, leading to the collection of mature oocytes.
Next, fertilization takes place via either traditional insemination or Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into an egg. Subsequently, embryos develop over a few days before being transferred into the uterus in hopes of achieving pregnancy. If IVF is successful, a pregnancy test is typically conducted two weeks after embryo transfer to confirm viability.
Understanding the IVF Age Cut-Off
One of the most critical factors influencing IVF success rates is the age of the prospective mother. Age is a reliable indicator of ovarian reserve and egg quality. As women age, especially beyond 35, the quantity and quality of their eggs diminish considerably, which can lead to decreased chances of conception. Thus, fertility specialists often implement a cut-off range based on age to maximize successful outcomes.
Research suggests that the ideal age for IVF is between 20 and 35 years. Women in this bracket tend to have optimal ovarian function, yielding higher success rates. However, as women age past 35, the success rates begin to decline decidedly. At 40, the likelihood of achieving a successful pregnancy through IVF is significantly lower. Some clinics may have strict policies regarding age, often imposing hard cut-off points at 44 or 45 years due to increased health risks for both the mother and child.
What to Consider Before Proceeding with IVF
Undergoing IVF is not merely a procedural decision; it entails emotional, physical, and financial considerations. Therefore, potential candidates must deliberate various aspects meticulously.
1. Medical Assessment: Prior to commencing IVF, a comprehensive fertility evaluation is paramount. This typically includes blood tests to assess hormonal levels, imaging studies like ultrasounds, and possibly semen analysis for male partners. Understanding the underlying causes of infertility can inform the tailored approach of the IVF protocol.
2. Emotional Readiness: The psychological toll of infertility and the IVF process itself cannot be overstated. Emotional readiness is essential, as candidates may undergo numerous cycles before achieving success. Support from mental health professionals or support groups can provide invaluable guidance during this tumultuous journey.
3. Financial Implications: IVF is a significant financial investment, often not covered by insurance. Costs can vary widely based on geographic location, clinic reputation, and specific treatment protocols. Furthermore, additional expenses may arise for medications, lab fees, and potential genetic testing of embryos. Exploring financing options or grants may alleviate some financial burdens associated with the procedure.
4. Understanding Success Rates: Success rates for IVF vary based on several factors, including age, health status, and specific fertility issues. It is crucial to explore clinic-specific statistics and not rely solely on general averages. Asking potential clinics about their experience with similar cases can provide insight into probable outcomes.
5. Potential Risks and Complications: IVF is generally safe; however, like any medical procedure, it carries certain risks. These can include ovarian hyperstimulation syndrome (OHSS), which occurs when the ovaries become overly stimulated, leading to swelling and discomfort. Additionally, multiple pregnancies significantly increase the risk of premature labor and other complications.
Navigating the IVF Experience
Once the decision to pursue IVF has been made, candidates must engage thoroughly in the process. This includes adhering to prescribed medications, attending regular monitoring appointments, and being transparent with healthcare providers about any concerns or unexpected feelings.
Embryo selection can also be a significant aspect to consider. Advances in preimplantation genetic testing allow prospective parents to screen embryos for genetic abnormalities, which can greatly influence the likelihood of a successful pregnancy. While this adds complexity, it is essential for resolving potential inherited conditions.
Conclusion: Evidence of Hope and Resilience
IVF is not merely a scientific endeavor; it encapsulates the dreams of individuals wishing to create or expand their families. While the age cut-off for IVF plays a vital role in determining eligibility and success, it is one of many factors that intertwine to shape the experience. Being informed, prepared, and emotionally equipped can pave the way for enduring success on this extraordinary journey.
As you consider embarking on the path of IVF, challenge yourself to confront your apprehensions, ask pertinent questions, and embrace the collective support available. The quest for parenthood is profoundly personal and transformative, beckoning you to explore its possibilities with an open heart and mind.